Standard Process & MediHerb
Leaders in Whole Food Supplements & Herbal Products
|
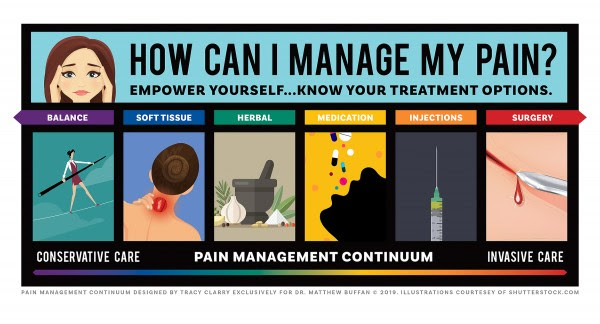
The last couple of months we've introduced the Pain Management Continuum:

This month we are focusing on using whole food supplementation and herbal remedies to support the soft tissue treatment we offer at our clinic.
|
Why Standard Process & MediHerb?
"Healthy Soil. Healthy Planet. Healthy Lives.
Standard Process is a Wisconsin-based family-owned company dedicated to making high-quality and nutrient-dense therapeutic supplements for three generations.
We apply a wholistic approach to how we farm, manufacture and protect the quality of our products. This comprehensive approach ensures that our clinical solutions deliver complex nutrients as nature intended. It's how we define the whole food health advantage." - Standard Process, Website
"MediHerb products are developed by experts and leaders in the field of herbal therapy, drawing on the latest scientific evidence, as well as centuries of traditional knowledge. The positive health results achieved are the strongest possible evidence of their potency and superiority." - Standard Process, Website
|
BOSWELLIA COMPLEX
Key Benefits
What it Supports
|
TURMERIC FORTE
Key Benefits
What it Supports
|
HEMP OIL COMPLEX
Key Benefits
What it Supports
|
Our focus in the office is on providing the best results for each individual patient. Often I hear the question "What can I do at home?" There are options to be done at home to support a healing environment from the inside. Many people live in a chronic state of inflammation and overuse. Pain limits life and is the opposite of fun. When there is pain, there is an inflammatory response.
If you prefer "nature first, drugs last" yet do not know where to start our office has advanced training in supporting your body. Chronic pain, advanced degeneration, and long term optimal health all require expert treatment, expert exercise instruction, and understanding a healing environment. We provided your functional solutions!
Achieve "Freedom From Pain", let us provide your natural functional solution to your goal.
Call 585-678-1362 today to speak with our team and get scheduled for your initial consultation.
Your Movement Matters,
Dr. Matt Buffan
|









 This month we are focusing on one of the most common, yet under diagnosed, causes of pain.
This month we are focusing on one of the most common, yet under diagnosed, causes of pain.